New Delhi
About 20-30% of my adult patients suffer from chronic constipation.
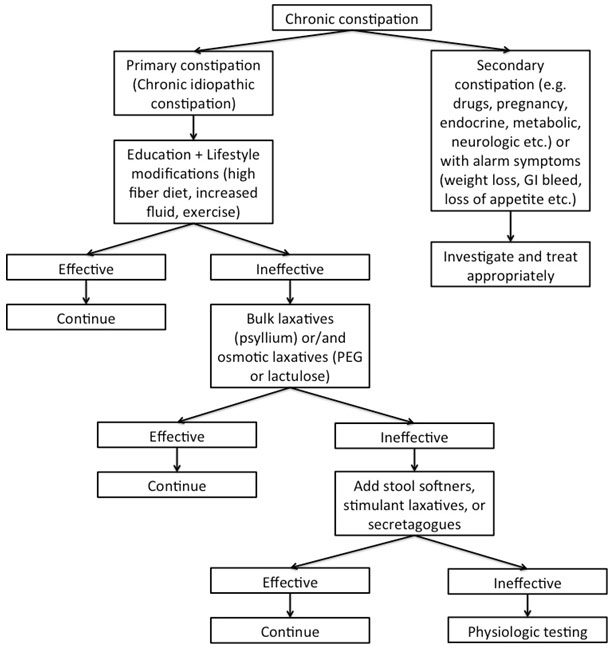
Chronic idiopathic constipation is a frequent complaint in my current practice. Notwithstanding the availability of numerous drugs, its treatment still remains unsatisfactory. The diagnosis of chronic idiopathic constipation can be made using standard criteria, and in the absence of alarm signs or symptoms, a determination of the underlying etiology can be gleaned from the history and physical examination alone. Specialized diagnostic testing may be warranted after the failure of initial laxative trials. Many therapeutic classes of laxatives exist however;I generally prefer to recommend over-the-counter therapies as the first line treatment while, using the prescription drugs only in patients who do not respond to the first line over-the-counter medications.
When lifestyle modifications do not work, multiple classes of agents can be tried for treating chronic constipation: bulking agents, stimulant and osmotic laxatives, stool softeners, emollients, secretagogues, and serotonergic agents. Each of these agents works via a specific mechanism of action. The first line agents are usually bulking agents (like fiber) and osmotic laxatives.
Chronic constipation requires long-term treatment. Lifestyle modifications (like increased dietary fiber intake, increased fluid intake and increased physical activity)should be advised for life. Bulk laxatives(like psyllium) and osmotic laxatives (like lactulose) can also be prescribed for long-term. Other medications like senna or bisacodyl etc. are generally prescribed for 2-3 weeks only depending on response and need of the patient.
Polyethylene glycol (PEG) is an osmotic laxative that is not absorbed by the small intestine, and maintains high osmotic pressure in the colon. Thus, it exerts its effect by driving water into the lumen. Well-designed studies on chronic constipation have shown that PEG is effective in improving stool frequency, consistency, and straining during defecation. In addition, PEG use in patients with chronic constipation for 6 months or more, was not associated with any serious adverse events. PEG is also able to alleviate constipation symptomsin patients with irritable bowel syndrome (IBS) with constipation IBS (C).PEG can be valued as a first-line drug for constipation.
The clinical efficacy of PEG has been proved in multiple studies. In the largest and longest laxative trial to date, 304 patients were randomized to receive PEG (n=204) or placebo (n=100) for 6 months (DiPalma et al, Am J Gastro, 2007).At completion of the study, individuals in the PEG cohort experienced a significant increasein bowel movements per week compared with placebo (7.9 vs 5.6; P<0.001) and thepercentage of individuals achieving a goal of 3 or more bowel movements per weekwas also significantly greater in favor of PEG (52% vs 11%; P<0.001). In addition, multiplemeta-analyses have also consistently yielded positive results favoring the use of osmoticagents. Ford and Suarez (Gut, 2011) recently pooled 5 studies comparing PEG and lactulosewith placebo and found that osmotic laxatives were significantly superior to placebo. Similarly, Belsey and colleagues (Int J ClinPract, 2010) analyzed 10 studies and found that PEG wassuperior to placebo and lactulose for increasing stool frequency.
PEG and lactulose, both are osmotic laxative, however, according to current evidence, PEG seems to be superior to lactulose. In a Cochrane meta-analysis by Lee-Robichaud et al published in 2010, it was found thatPEG is better than lactulose in outcomes of stool frequency per week, form of stool, relief of abdominal pain and the need for additional products. Thus it was concluded that PEG should be used in preference to lactulose in the treatment of chronic constipation.
PEG and ispaghula (psyllium), both have different mechanism of actions. While PEG is an osmotic laxative, ispaghulais a bulking agent. Although both can be used as first line agents in treatment of chronic constipation, PEG may have slightly superior efficacy. Since they have different mechanism of actions, both can be combined in patients who do not respond to either agent alone.
Both PEG and lactulose are osmotic laxatives and are strongly recommended by the American College of Gastroenterology (ACG) for the treatment of chronic constipation; however, current literature suggests that the efficacy of PEG is higher than that of lactulose for treatment of chronic constipation.
Constipation predominant irritable bowel syndrome or IBS (C) is a common disorder. Similar to chronic idiopathic constipation, IBS(C) is also included among the functional bowel disorders, and has a significant personal, healthcare, and social impact, affecting the quality of life of the patients who suffer from it. In IBS (C), constipation represents the predominant complaint, in association with recurrent abdominal pain, bloating, and abdominal distension. There are many clinical and pathophysiological similarities between IBS (C) and chronic idiopathic constipation, and both respond similarly to common drugs, their primary difference being the presence or absence of pain. Treatments for chronic constipation and IBS (C) differ, but symptom criteria do not reliably distinguish between them; some regard chronic idiopathic constipation and IBS (C) as parts of a single constipation spectrum.
PEG is useful in patients with IBS (C). In a recent randomized controlled trial by Chapman et al (Am J Gastro, 2013) it was found that in IBS-C, PEG was superior to placebo for relief of constipation, however it did not lead to a significant improvement in abdominal discomfort/pain. Thus PEG can be considered suitable for use in IBS (C) as adjunctive treatment.
An algorithmic approach should be followed for treating patients with chronic constipation. A simple algorithm is given below: